The development of clogged arteries, a hallmark of atherosclerosis, is a growing concern for women turning 40 and beyond, entering the menopausal phase.
Recognizing the urgency of this issue, it becomes crucial for women to adopt strategies that can prevent the progression of this disease from an early stage.
One such strategy is using hormone replacement therapy with oral estradiol pills.
Find out how by harnessing hormone therapy, women can take proactive measures to safeguard their heart health and mitigate the risks of atherosclerosis.
Hormone Therapy With Oral Estradiol Pills Can Put the Brakes on Atherosclerosis

Caring for Heart Health During Menopause: Why It Matters
Women should be concerned about their heart health before they reach menopause due to the significant role estrogen plays in maintaining cardiovascular well-being.
Estrogen, a hormone produced by the ovaries, has cardioprotective properties contributing to heart health. It helps keep heart tissues healthy by promoting the dilation of blood vessels, reducing inflammation, and preventing blood clots.
However, as women approach menopause, estrogen levels decline. Low estrogen has substantial implications for the heart and cardiovascular system. Thus, the absence of estrogen’s protective effects may increase the risk of developing heart disease, including atherosclerosis, high blood pressure, and coronary artery disease.
It becomes crucial for women to pay close attention to the rhythm of their hearts and adopt preventive measures such as maintaining a healthy lifestyle, eating a balanced diet, engaging in regular exercise, and, most importantly, seeking medical guidance.
Women! The clock is ticking, and your heart’s defense cannot wait.
Hormone Replacement Therapy and Heart Health
Hormone replacement therapy (hormone therapy or HRT) emerges as a game-changer in postmenopausal heart health, with studies providing evidence of its benefits.
Notably, Hodis H. et al.’s groundbreaking research demonstrates hormone therapy’s profound positive impact on heart disease prevention.
Their findings reveal that estrogen, with or without progestogen, statistically reduces the risk of heart disease by a staggering 52% after a decade of treatment. This remarkable reduction in risk holds promise for women grappling with menopause.
By considering hormone therapy as a preventive strategy, women can safeguard their hearts from disease and simultaneously lower the risk of all-cause mortality and other age-related conditions. Hormone therapy is, therefore, a transformative approach that has the potential to enhance overall well-being and extend a woman’s health span.
However, while hormone therapy has shown evidence of its benefits in preventing heart disease, further research has explored the varying clinical outcomes based on different initiation timings. This premise has led to the hormone-timing hypothesis, which emphasizes the importance of timing when implementing hormone therapy.
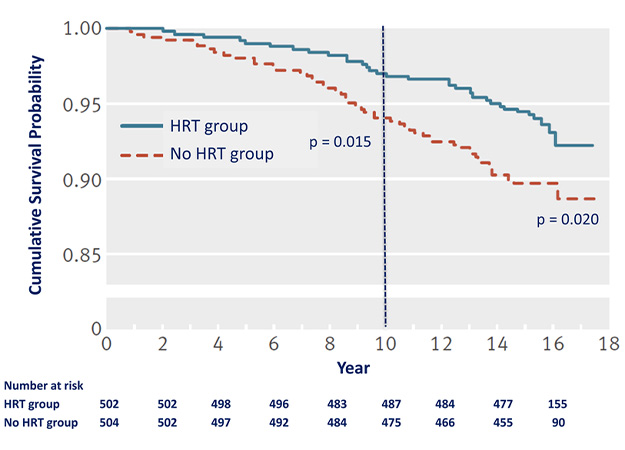
After 10 years of hormone replacement therapy, the survival curve shows a 52% decrease in cardiovascular disease.
Understanding the Hormone-timing Hypothesis
The hormone-timing hypothesis refers to the role of timing of hormone therapy regarding cardiovascular outcomes, in which atherosclerosis is the primary concern.
This hypothesis exists as the same study by Hodis H. et al. points out the divergent clinical outcomes associated with different initiation times of hormone therapy, specifically focusing on oral estradiol pills, alone or in combination with progestogen.
Specifically, women who began hormone therapy within six years of menopause showed remarkably positive cardiovascular outcomes, as evidenced by a carotid intima-media thickness (CIMT) of slightly over 0.7 mm after an average of five years of intervention. This CIMT measurement falls within the range considered healthy and normal.
In stark contrast, those who initiated hormone therapy ten or more years after menopause already had a significantly worse CIMT score at the commencement of treatment. After five years of intervention, their CIMT readings exceeded 0.8 mm, placing them dangerously close to a high risk of cardiovascular disease.
These findings underscore the importance of the hormone-timing hypothesis in optimizing heart health outcomes. Acting swiftly within the critical time window (ideally less than 6 years past menopause) can potentially preserve the integrity of the cardiovascular system and mitigate the risks associated with menopause.
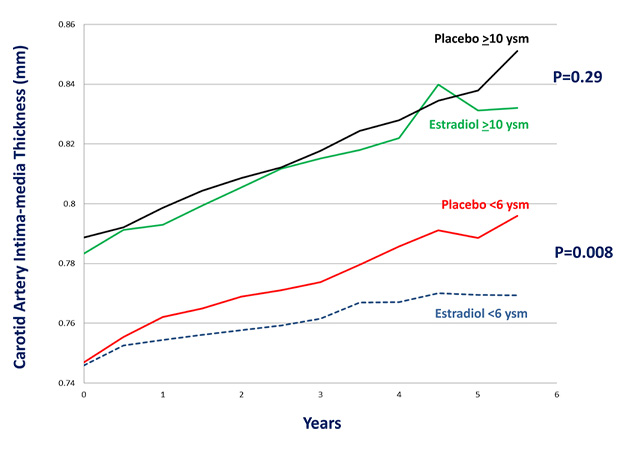
The effect of hormone therapy on atherosclerosis progression differed between women starting the treatment less than 6 years and 10 or more years past menopause.
Early Prevention of Heart Disease With Hormone Therapy
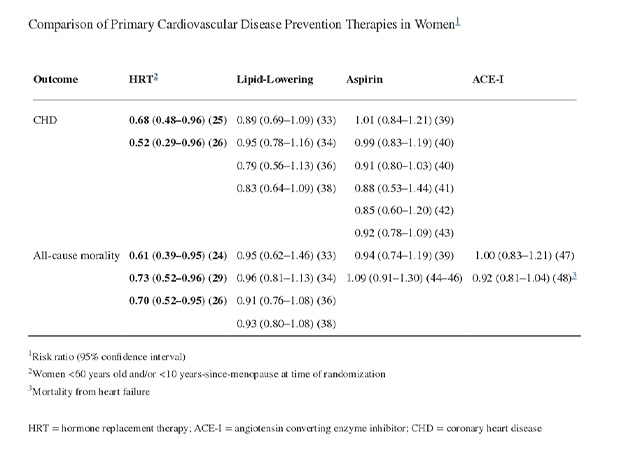
Comparing different therapies’ clinical benefits is a common approach to understanding their effectiveness. In the case of hormone therapy with oral estradiol pills, it is no exception. Hodis H. et al. evaluated the therapy’s role as a preventive strategy compared to other medications in cardiovascular disease (CVD) prevention.
Lipid-lowering medications, particularly statins, are often the mainstay for CVD prevention in women and provide an appropriate point of comparison for hormone therapy.
A meta-analysis evaluating lipid-lowering therapy showed that it did not significantly reduce the risk of having coronary heart disease (CHD), nonfatal myocardial infarction (MI), or CHD mortality. However, it reduced these conditions’ outcomes by 20-30%.
However, statin therapy did not reduce all-cause mortality in women for primary prevention. This pattern was observed even in cohort studies involving thousands of women.
In comparison, hormone therapy with oral estradiol pills initiated under 60 significantly reduced all-cause mortality and CHD by 30-50%. This finding contrasts lipid-lowering therapy, aspirin, and ACE inhibitor therapy, which did not substantially affect CHD, with all-cause mortality rates ranging from 0.91 to 1.09.
Comparison of cardiovascular disease prevention therapies in women.
Bottom Line
With the power of hormone therapy at their disposal, women can rewrite the narrative of their postmenopausal health, empowering themselves with a potent tool that transcends cardiovascular protection and promises a healthier, vibrant future.
Meanwhile, the hormone-timing hypothesis serves as a poignant reminder that the timing of hormone therapy initiation with oral estradiol pills may be a determining factor in the overall effectiveness of the treatment, particularly with heart health.
Healthcare providers must consider individual risk profiles and the time elapsed since menopause when recommending hormone therapy options, enabling women to make informed decisions that maximize the benefits and minimize risks.
References
Hodis H. et al. (2022). Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease: It’s About Time and Timing.
Yunique Medical provides FUNCTIONAL MEDICINE for optimized health and performance. We offer customized, scientifically advanced treatments to create a new state of human thriving. Why be ordinary when you can be optimal?
HUMAN 2.0 begins here!
Contact us to schedule your FREE consultation at one of our three locations in Florida – Ocala, Fruitland Park (The Villages), and Daytona.
UP NEXT: