Breast Cancer Screening: Why Choosing the Right Screening Test Matters
According to the National Cancer Institute (NCI), for American women, breast cancer ranks as the second most common cause of cancer-related deaths. Skin cancer is the only cancer type that affects women more frequently than breast cancer in the US.
By catching cancer at its earliest stages, women not only increase treatment success but also reduce the need for aggressive interventions.
Explore how women can detect potential breast cancer and implement appropriate treatment through breast cancer screening. Also, learn which screening test is best for prompt and accurate diagnosis.

Adopting an Appropriate Screening Test is the Key to Early Diagnosis of Breast Cancer
Why is Breast Cancer Screening Important?
Early Detection & Better Prognosis
If caught in its initial stages, breast cancer is often treatable and has a better prognosis. Women must understand the significance of regular breast cancer screening, as it offers the best chance of detecting abnormalities before they escalate into a full-blown, fatal disease.
Increased Treatment Success Rates
The importance of breast cancer screening lies in its ability to identify tumors or irregularities in breast tissue long before symptoms manifest. Early detection increases treatment success rates and opens up less invasive and more manageable intervention options.
Less Impact of Aggressive Treatments
Moreover, breast cancer is notorious for its asymptomatic nature in the initial stages. When symptoms become noticeable, the disease may have progressed to an advanced and more challenging stage. Regular screening acts as a preemptive strike, providing an opportunity to catch cancer at its most vulnerable state – when it’s small, localized, and easier to eradicate.
When Should Women Start Breast Cancer Screening?
Experts agree that early breast cancer screening age is critical and recommend that women should start regular breast cancer screening at the age of 40.
However, individual risk factors can alter this recommendation.
For women with a family history of breast cancer (first-degree relatives, such as a mother or sister) or those with the presence of BRCA gene mutations (BRCA1 or BRCA2 genes), screening might need to commence earlier.
Tailoring the screening approach to individual risk profiles ensures that high-risk individuals are identified and monitored more closely.
Screening intervals are another crucial aspect. Annual mammograms are advised for women over 40, but again, personal and familial risk factors may influence the frequency of screening. Establish a proactive dialogue with your healthcare provider to devise a screening plan that aligns with your circumstances.

Which Screening is Used to Test for Breast Cancer?
Mammogram for Breast Cancer Screening
Mammography is the cornerstone of breast cancer detection. This X-ray imaging method captures images of the breast to identify abnormalities such as tumors or cysts.
While discomfort may be associated with breast compression during the procedure, the benefits far outweigh the temporary inconvenience.
Each breast is compressed between two plates during a mammogram, while low-dose X-rays are used to create detailed images.
Digital mammography has become increasingly common, offering enhanced image quality and the ability to manipulate and store images more efficiently.
Ultrasound for Breast Cancer Screening
Ultrasound imaging utilizes high-frequency sound waves to create detailed images of the breast’s internal structures.
This method is particularly useful in distinguishing between solid masses and fluid-filled cysts. It’s safe, non-invasive, and doesn’t involve ionizing radiation.
During the procedure, a gel is applied to the breast, and a transducer is moved over the skin, emitting sound waves that bounce back and create images on a screen.
Ultrasound is often a supplementary tool when further evaluation is required following a mammogram or clinical breast exam (CBE).
MRI for Breast Cancer Screening
Magnetic Resonance Imaging (MRI) is a powerful technique that uses a magnetic field and radio waves to generate detailed images of the breast.
MRI is especially valuable for detecting cancer in women at high risk or with dense breast tissue. Like ultrasound, MRI doesn’t use X-rays or radiation.
The procedure involves the patient lying face down on a platform with breasts positioned into openings in the table. A contrast agent may be injected to enhance image quality.
The MRI then creates detailed cross-sectional images of the breasts, providing a comprehensive view of breast tissue.
Thermography for Breast Cancer Screening
Thermography involves using infrared cameras to detect heat patterns and blood flow in the breast. The premise is that cancer cells often generate more heat than normal cells.
While it’s a non-invasive and radiation-free option, its effectiveness as a stand-alone screening tool remains controversial within the medical community.
During a thermography session, the patient stands in front of an infrared camera, which captures temperature variations on the breast’s surface.
Although thermography has potential, it’s usually used as a supplementary tool rather than a primary screening method.
Which Breast Cancer Screening Method is the Best?
Choosing the best breast cancer screening method involves a careful consideration of the advantages and disadvantages of each approach.
While no single method is universally superior, certain factors may influence the choice based on individual circumstances.
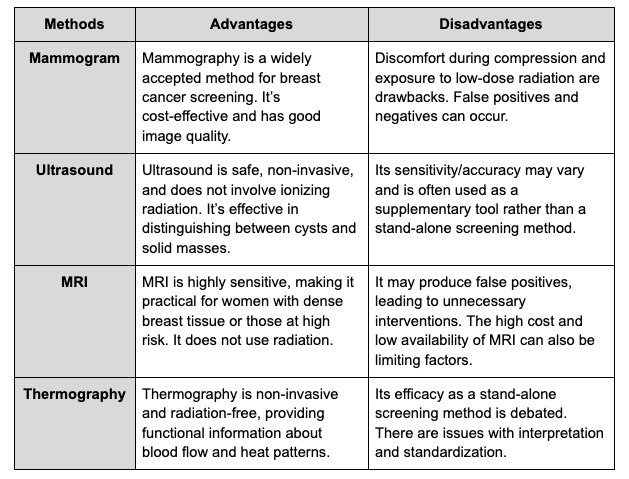
Comparison:
While each method has advantages, mammography is the most established and widely utilized screening tool. Its efficacy, cost-effectiveness, and established track record make it the standard method in breast cancer screening programs.
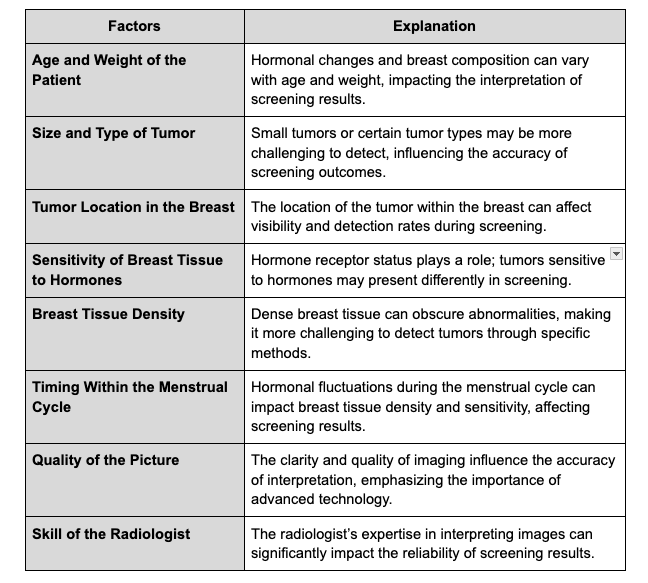
What Factors Affect the Results of Breast Cancer Screening?
The accuracy and reliability of breast cancer screening results can be influenced by various factors, including:

Do the Benefits of Screening Outweigh the Risks?
False Positive Test Results
While breast cancer screening is crucial, false-positive results can lead to unnecessary anxiety and medical interventions. Even though no cancer is present, a woman may face the distress of a positive diagnosis. Seeking a second opinion from a different pathologist is time-consuming, adding to the emotional burden.
The chance of a false-positive result increases with more screening tests. Confirming a correct breast cancer diagnosis avoids unnecessary treatments and psychological strain.
False Negative Test Results
On the flip side, false-negative results pose a severe risk. If a screening test fails to detect cancer, a woman may mistakenly believe she’s free from the disease, leading to a delay in seeking medical care even if symptoms arise. A missed cancer diagnosis can result in more advanced disease stages and decreased treatment success.
Overdiagnosis and Overtreatment
Overdiagnosis, the detection of cancers that may never pose a threat, can lead to unnecessary and unwanted side effects of aggressive treatments.
Treating non-threatening cancers exposes individuals to the risks and burdens of interventions without corresponding benefits.
Exposure to Radiation
Mammography exposes women to low-dose radiation, causing discomfort and pain during procedures. Repeated X-rays over time raise concerns about cumulative radiation exposure.
While the benefits of early cancer detection are substantial, it’s essential to weigh these against the potential harms associated with radiation exposure during routine screening.
Bottom Line
Screening for breast cancer isn’t a mere option; it can mean the difference between life and death. In the battle against breast cancer, early detection is our most potent weapon. When time is often the decisive factor in overcoming breast cancer, the urgency of embracing screening tests cannot be overstated.
Breast cancer screening is more than just about extending life; it’s about preserving the quality of that life by minimizing the impact of aggressive treatments.
Yunique Medical provides FUNCTIONAL MEDICINE for optimized health and performance. We offer customized, scientifically advanced treatments to create a new state of human thriving. Why be ordinary when you can be optimal?
HUMAN 2.0 begins here!
Contact us to schedule your FREE consultation at one of our three locations in Florida – Ocala, Fruitland Park (The Villages), and Daytona.
UP NEXT:

