Menopause rewrites the rules for sleep, mood, strength, and bone health. For years, hormone therapy was treated with suspicion, but the science has shifted. Modern data shows it calms symptoms, protects bone, and supports metabolic health when started in the right window and delivered the right way.
The key is precision.
Your biology, history, and goals guide the plan — not a template.
This article breaks down what hormone therapy really does, what the evidence shows, and how personalization changes the outcome.
TL;DR: MHT Works When It’s Timed and Personal
- Hormone therapy is the most effective way to calm hot flashes, improve sleep, and relieve dryness. It also protects bone, and protection fades once therapy stops.
- Starting within 10 years of menopause, or before age 60, is linked with better results for symptoms, bone, and heart health.
- Patches and gels deliver estrogen through the skin, which avoids the liver, lowers clotting risk, and shows better metabolic and liver signals than pills.
- Some studies show less buildup of tau and amyloid in women on therapy, but the evidence is not strong enough to use HRT for dementia prevention alone.
The Science Has Moved On (and It’s Good News)
1. Bone strength and fracture reduction
Your bones thin quickly after menopause (about 10% in the first five years), which is why everyday falls start turning into broken wrists or hips. But personalized hormone therapy can steady that loss and help bones hold their strength.
In the Women’s Health Initiative trials, women on therapy had higher bone density and fewer fractures across every risk group. Long-term follow-up confirmed another signal: estrogen alone not only protected bone but also lowered breast cancer incidence and mortality.
The protection only lasts while therapy continues. Once it stops, bone density begins to decline again.
2. Cardiovascular and metabolic signals (when started early)
Starting hormone therapy within about 10 years of menopause, or before 60, is linked with better heart and vascular health. Women who begin in that window show better blood pressure, cholesterol, and vessel changes, with lower overall mortality in long-term reviews.
A 2020 systematic review pulled together data from both trials and observational studies.
Observational research suggested women on hormone therapy had fewer heart attacks, especially when treatment started earlier. Randomized trials did not show that same drop, in part because they enrolled older women long past menopause who already carried more heart disease.
The review also made one risk clear: clotting. Both data sets linked oral estrogen to higher rates of blood clots and pulmonary embolism. Patches and gels that deliver estrogen through the skin showed a safer profile, with lower clotting risk
Metabolic health follows the same trend: in women with prediabetes, therapy was tied to a lower chance of developing diabetes over 20 years.
The key is timing. Early use is where the benefits show up most clearly.

3. Brain health — what looks promising
Researchers have studied how hormone therapy affects proteins that drive Alzheimer’s disease. Two of the biggest culprits are tau and amyloid-β: Tau forms tangles inside brain cells, and amyloid-β forms plaques between them. Both build up years before memory symptoms appear.
Women on therapy have shown lower levels of these proteins on brain scans and blood tests.
The clearest signal shows up in women with APOE ε4, a gene that raises Alzheimer’s risk. In one cohort study, women using transdermal estradiol had less amyloid buildup than those not on therapy.
Real-world results are harder to pin down. One large study of older women with breast cancer found fewer dementia diagnoses in those on therapy, but other trials have not confirmed it.
That’s why we don’t prescribe HRT to prevent dementia. Right now, hormone therapy’s job is to steady symptoms, protect bone, and support the body’s overall resilience.
4. Strength and body composition
After menopause, it gets harder to hold onto muscle, and the loss shows up in everyday strength — climbing stairs feels heavier, workouts give less return, and recovery takes longer.
A randomized trial tested whether hormone therapy could shift that balance. Women who used transdermal estradiol while doing resistance training gained more lean muscle than those who trained without it.
The signal here is not about estrogen alone — it works best when paired with strength training and adequate protein. Hormone therapy creates the environment, but the muscle only grows with work and fuel.
5. Route matters (and why we often favor transdermal)
The way estrogen enters the body makes a difference.
Pills move through the gut and into the liver first, which raises clotting factors and strains liver metabolism. Patches and gels move through the skin instead, skipping the liver’s first pass.
A systematic review linked oral estrogen with more clotting events, while non-oral routes showed a safer profile.
Women on oral therapy were more likely to develop non-alcoholic fatty liver disease (NAFLD). Women on transdermal therapy were less likely, suggesting a protective effect.
Transdermal routes take clotting and liver strain off the table while still keeping symptoms under control. That’s why patches and gels often end up as the first choice.
Personalization > Templates: How YM Builds Your Plan
Listen and baseline
Every plan starts with your story, not a lab slip. We map your symptoms, trace your medical history, and sort through risk factors. Hot flashes, poor sleep, or brittle bones each point in different directions, and knowing which ones drive the picture sets the tone for your plan.
Test smart
We don’t shotgun labs. We order what shifts the decision. Hormones, glucose, inflammatory markers, and liver function show how your system is running. If bone strength is at stake, we add a DEXA scan for a clear baseline. Testing is a tool, not a ritual.
Choose your route and dose
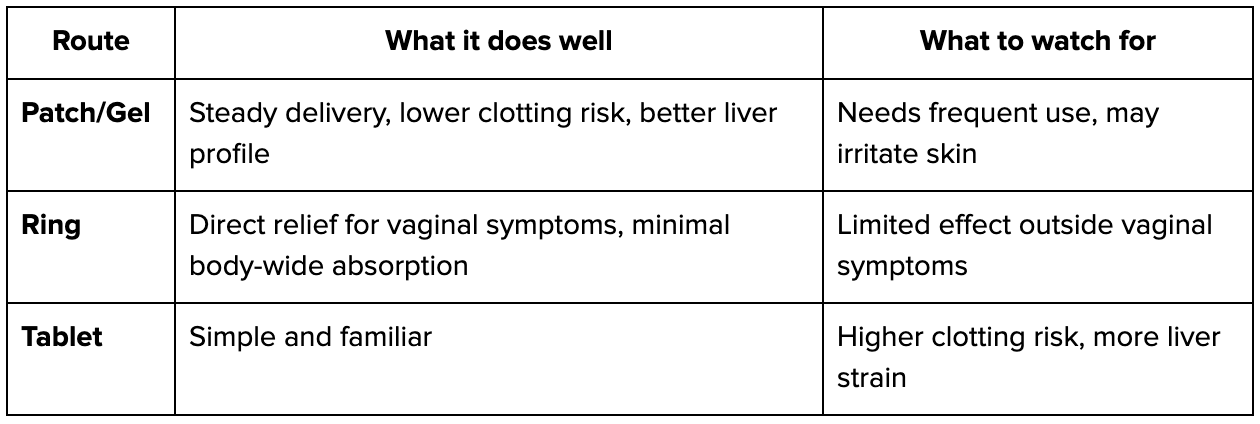
How estrogen enters the body changes the outcome. Pills move through the gut and liver, which raises clotting factors and strains metabolism. Patches and gels deliver through the skin and bypass that first pass. Rings act locally for dryness but won’t touch bone or muscle.
The right route comes from your biology, your risks, and your goals.
Set lifestyle anchors
Hormones don’t build strength on their own. We lock in protein targets, resistance training, and a sleep plan. Without those anchors, even the best prescription runs flat.
Follow up and adjust
Your biology shifts, so the plan shifts with it. We track symptoms week to week, recheck labs, and score energy, sleep, and recovery. Dose and route change when the data calls for it.

Who’s a Good Candidate? (And Who Should Pause or Consult)
Most benefits and the best safety profile show up when women start menopausal hormone therapy before age 60 or within about 10 years of their final period. Evidence links that window with better cardiovascular outcomes and lower overall mortality compared with later starts.
Good candidates
The best window is early. Women under 60, or within about 10 years of menopause, see the strongest benefits and the safest profile.
- under 60 or within ~10 years of menopause
- hot flashes or night sweats disrupting daily life
- broken sleep or persistent fatigue linked to symptoms
- vaginal dryness or urinary symptoms
- need for bone protection in the face of early bone loss
Pause or consult first
When these are on the table, therapy isn’t off-limits forever, but it does mean stopping to investigate and sometimes pulling in a specialist before moving ahead.
- Active or recent hormone-sensitive cancer: Coordinate with oncology before any therapy.
- Unexplained vaginal bleeding: Evaluate the cause before starting.
- History of blood clots (VTE/PE) or stroke: Review risks, routes, and alternatives with a specialist.
- Known clotting disorders or severe liver disease: Get targeted evaluation and consider non-oral routes only if cleared.
- High, uncontrolled cardiovascular risk: Optimize blood pressure, lipids, and glucose first, then reassess timing and route.
What we check before starting
We run through your history first. That means your own medical background, your family’s patterns, the medications you take, and any past clotting events. We measure blood pressure, cholesterol, and glucose to see how your system is handling risk today. If we need to know about bone strength, we order a DEXA scan and set a clear baseline.
Those results drive the next step. A clotting history points us to a patch or gel. Rapid bone loss pushes us to act sooner. The data tells us where to start and how to dose, and we build the plan from there.

FAQ: Straight Answers, No Spin
1. Does HRT cause breast cancer?
Estrogen alone, in long-term WHI follow-up, was linked with lower breast cancer rates and lower mortality. Combined therapy has a different risk profile, so the decision depends on history and goals.
2. Isn’t clot risk a deal-breaker?
Clotting risk is real, but it depends on health history and route. Oral estrogen carries more of it. Patches and gels bypass the liver and consistently show a safer profile.
3. Can HRT prevent dementia?
No. Some studies show better brain markers — less tau and amyloid buildup, especially in women with the APOE ε4 gene — but outcomes are mixed. We use HRT to treat symptoms, protect bone, and support resilience, not to prevent dementia.
Why Yunique Medical vs. a Template Clinic?
Because your plan isn’t copy-pasted. We match route and dose to your biology, set realistic lifestyle anchors, and adjust based on labs and symptoms. The follow-up is built in, not an afterthought.
Ready to Feel Like Yourself Again?
Menopause shifts the way your body runs — sleep, energy, and strength all start to play by new rules. Hormone therapy can help, but it only delivers when the plan is built around your whole system. That means tracking bone, metabolism, recovery, and the way your body responds over time.
The aim isn’t short-term relief. The aim is long-term resilience that carries you through the decades ahead.
Our Services
We offer a wide range of services to support your wellness journey, including:
- Hormone Optimization
- Infusion Therapy
- Weight Loss Programs
- Cellular & Functional Medicine
- Precision Longevity
- HeartFit Program
- Sexual Enhancement
- Peptide Therapy
- HOCATT Biohacking
Our Locations
You can find us here:
- Port Orange, FL
- Lady Lake, FL (formerly Fruitland Park Office)
- Ocala, FL
Schedule a 30-minute consult with our team, or start with the 2-minute YM Menopause Quiz to see if you’re in the right window.


