We do NOT answer medical questions online or via text. We do NOT sell individual peptides. Our clinical peptides are available only through our optimization and longevity programs.
Your first infusion session is usually easier than you imagine. The sharpest moment is the quick pinch of the IV needle during placement. After that, most of what you’ll notice is the waiting.
Infusion rooms are designed to be calm, and nurses are skilled at keeping you comfortable while the medication runs. Every step, from scheduling the appointment to finishing the session, is overseen by trained medical professionals.
This guide breaks down what to expect the first time — how to prepare, what happens during the session, how long it lasts, and which side effects are normal — so there are no surprises.
How Do I Prepare for Infusion Therapy?
Preparing for your first infusion is simple: eat beforehand, stay hydrated, dress for comfort, and bring items that make the time easier.
1. Eat a Light Meal
Have a simple breakfast or lunch with protein and complex carbs. It keeps your blood sugar steady, lowers nausea risk, and prevents dizziness. Avoid heavy or greasy foods that can upset your stomach during the session.
2. Stay Hydrated
Drink water throughout the morning and bring a water bottle with you. Hydration helps nurses place the IV more easily and reduces post-infusion fatigue. Limit caffeine, which can dehydrate and make you jittery.
3. Dress for Comfort
Choose loose sleeves for IV access and bring layers in case the room feels cold. Many clients bring their own blanket or warm socks for extra comfort. Think of it as packing for a long flight.
4. Bring Personal Items
Sessions often last several hours. A book, headphones, tablet, or even snacks (if allowed) help pass the time. Some clients also keep a small journal to track how they feel during and after treatment.

5. Ask About Medications
Double-check with your provider if any prescriptions, vitamins, or supplements should be paused. Write down your current medication list to bring with you.
6. Plan Your Ride
Even if you usually drive, arrange a backup ride for your first infusion. Some medications leave you too tired to drive safely. Having a family member or friend pick you up removes the stress of deciding afterward.
7. Pack for Comfort Breaks
Infusions can take hours, so plan for small breaks. Wear shoes you can slip on easily, and ask staff where the restroom is before your session starts.
8. Manage Anxiety Ahead of Time
If you’re nervous about needles or the process, let the nurse know right away. Many infusion teams use numbing sprays, relaxation techniques, or distraction methods to make the start easier.
What Happens During the Session?
Once you arrive, the infusion follows a set routine. Nurses guide you through check-in, place the IV, start the medication, and keep watch until it finishes. Most of the session is waiting comfortably while the drug runs at a steady pace.
- Check-in and vitals: Staff confirm your identity, review allergies, and record baseline vitals like blood pressure, temperature, and heart rate.
- IV placement: A nurse inserts a line, usually in your arm or hand. Most clients feel a quick pinch followed by mild pressure.
- Medication delivery: The infusion begins at a controlled pace, either through a drip or a pump.
- Monitoring: Nurses track your vitals, watch for reactions, and adjust the flow rate if needed.
- Passing the time: Many clients rest, read, or use personal devices while waiting for the infusion to finish.
How Long Does a Session Take?
Most sessions last several hours, and the first is often the longest because staff move slowly to check how your body responds.
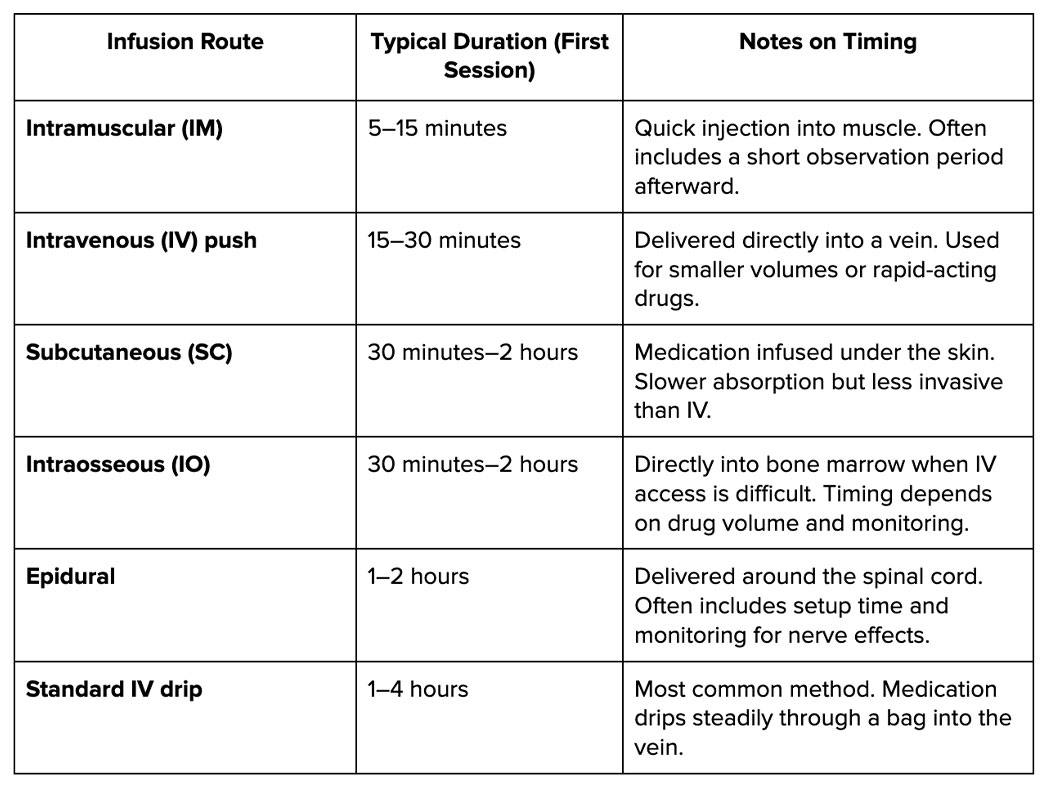
Your first infusion usually takes the most time. Nurses run the medication slowly and watch closely to see how your body reacts. Once you’ve had a safe first session and your team knows you tolerate it well, later infusions often move faster and fit more easily into your routine.
What Side Effects Should I Expect?
Most side effects during a first infusion are short-lived, like fatigue and a slight headache. But severe dizziness and chest pain warrant emergency care.
Common, Mild Effects and After-session Symptoms
These are the effects most people notice, and they usually fade within a few hours to a day:
- fatigue during or after the session
- mild headache
- nausea or stomach upset
- soreness or bruising near the IV site
- temporary flushing, chills, or metallic taste in the mouth
Red-Flag Reactions
Below are not typical and should be treated as urgent. If they happen during your infusion, call the nurse immediately. If they appear after you leave the center, contact your clinic or seek emergency care without delay:
- sudden rash or hives
- chest tightness or pain
- shortness of breath or wheezing
- severe dizziness or lightheadedness
Once your infusion ends, nurses keep you for a short observation period before you leave. Most medications require about 15 to 30 minutes, but some call for longer. During that time, your care team watches for delayed side effects and makes sure you’re stable. You only go home once they’re confident it’s safe.
FAQ: First Infusion Therapy Session
1. What should I expect at my first infusion?
Plan on checking in, having your vitals taken, and getting an IV placed. The medication runs slowly at first while nurses watch for side effects. Most of the session is simply waiting in a comfortable chair until the infusion finishes.
2. What not to do before IV infusion?
Avoid skipping meals or arriving dehydrated. Don’t start or stop medications on your own — always check with your provider first. Limit alcohol and caffeine the night before since both can make hydration and IV placement more difficult.

3. What to do while getting an infusion?
Use the time to rest. Read, watch a show, or listen to music. Stay hydrated if your nurse says it’s okay, and let staff know right away if you feel anything unusual, like dizziness, chest tightness, or itching.
4. What not to do after an infusion?
Don’t push yourself into strenuous activity right away, especially if you feel tired. Avoid driving if you’re drowsy or your provider advised against it. Skip alcohol for the day since it can worsen dehydration or nausea. Give your body time to recover.
What to Do Next
Your first infusion session may feel unfamiliar, but most clients find the process easier than they expected once they know the steps.
Preparing ahead of time, asking questions, and paying attention to how your body responds will help you move through treatment with more confidence.
Keep a simple record of how you feel during and after your session. Sharing that with your care team at the next visit helps them adjust the plan and make future infusions smoother.
How We Support Clients
At Yunique Medical, we focus on giving clients clarity about their health. That begins with advanced diagnostic testing, continues with personalized care planning, and extends into ongoing monitoring to track progress over time.
Our role is to connect the details of your biology with a plan that makes sense for your goals. Every step is designed to give you the information and support you need to move forward with confidence.
Our Services
We offer a wide range of services to support your wellness journey, including:
- Hormone Optimization
- Infusion Therapy
- Weight Loss Programs
- Cellular & Functional Medicine
- Precision Longevity
- HeartFit Program
- Sexual Enhancement
- Peptide Therapy
- HOCATT Biohacking
Our Locations
You can find us here:
- Port Orange, FL
- Lady Lake, FL (formerly Fruitland Park Office)
- Ocala, FL
Book a consultation and see how personalized planning can work for you.



