Hormones are vital chemical messengers in the human body. Without them, our bodies would not function normally and might fall into dysfunction and illness.
However, did you know that hormones can also be the cause of some diseases, like breast cancer?
Hormone therapy for breast cancer is what you need to stop, treat, and even prevent the development of these diseases.
RELATED: 5 Facts & Myths About Female Testosterone Replacement Therapy
Understanding Hormone Therapy for Breast Cancer
What Is Hormone Therapy for Breast Cancer?
Hormone therapy for breast cancer involves altering the activities and amounts of the estrogen hormone in the female body to treat breast cancer.
Hormone therapy for breast cancer should not be mistaken for menopausal hormone therapy (also known as hormone replacement therapy or HRT), which uses estrogen alone or in conjunction with progesterone to treat menopausal symptoms.
It is impossible to simultaneously prescribe menopausal hormone therapy and hormone therapy for breast cancer. Usually, a woman must stop menopausal treatment after receiving a breast cancer diagnosis and being prescribed hormone therapy for the disease.
How Does Hormone Therapy for Breast Cancer Work?
Blocking Estrogen Activities on Cancer Cells

The first mechanism by which hormone therapy helps treat breast cancer is that it blocks the receptors on the cancer cells from attaching to estrogen.
A receptor is a protein that can be activated when it’s attached to estrogen. If a cancer cell receptor and estrogen are bound, the activated receptor can cause changes in some genes, allowing estrogen to be the “fuel” that drives cancer growth.
Because hormone therapy inhibits the receptors enabling the activities between the cancer cells and estrogen, only women with cancer cells that have receptors (hormone receptor-positive cancer) should consider hormone therapy for breast cancer.
That said, about 2 out of 3 breast cancers (67–80%) are hormone receptor-positive. In contrast, women whose tumors don’t have hormone receptors (hormone receptor-negative cancer) cannot benefit from the therapy and should choose other treatments.
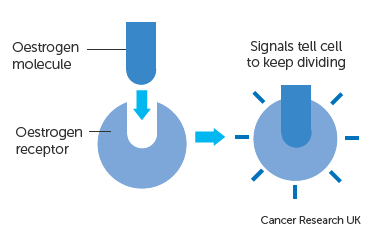
How an estrogen molecule is attached to an estrogen receptor of a cancer cell. Source: Cancer Research UK
Reducing the Body’s Production of Estrogen
Another mechanism is lowering the amount of estrogen produced by the female body to the point that estrogen cannot fuel breast cancer development.
As mentioned above, estrogen can promote the growth of breast cancer (hormone receptor-positive cancer). In healthy breast tissues, estrogen is involved in the development and function of normal cells. Unfortunately, if normal cells are turned cancerous for some reason, estrogen can cause cancer cells to multiply and spread.
RELATED: The Impact of Hormone Replacement Therapy on Menopause Symptoms
Types of Hormone Therapy for Breast Cancer
Medications That Block Estrogen Activities on Cancer Cells
| Medications | Types | Indications | Duration and side effects |
| Tamoxifen (Nolvadex) | Selective estrogen receptor modulator (SERM; anti-estrogen in breast cells, pro-estrogen in other cells) | Mainly for pre-menopausal women with early-stage breast cancer
Lower the risk of developing breast cancer Lower the risk of cancer coming back Slow or stop the growth of the cancer Oral. Taken either after or before surgery |
5 to 10 years
Hot flashes Vaginal dryness or discharge Changes in the menstrual cycle |
| Toremifene (Fareston) | Selective estrogen receptor modulator (SERM) | Used less often than Tamoxifen
Only approved to treat post-menopausal women with metastatic breast cancer Oral. Not likely to work if Tamoxifen has already been used and has stopped working |
5 years (long-term use is usually not recommended)
Side effects are similar to Tamoxifen |
| Fulvestrant (Faslodex) | Selective estrogen receptor degrader (SERD; attach to and break down estrogen receptors; anti-estrogen throughout the body) | Mainly for post-menopausal women with advanced breast cancer
Given alone to treat advanced breast cancer that has/has not been treated with other hormone therapy Injectable. Twice in the first month, 2 weeks apart, then once a month. |
As long as it keeps breast cancer under control
Hot flashes Night sweats Headache Mild nausea Bone pain Injection site pain |
Medications That Reduce the Body’s Production of Estrogen
| Medications | Types | Indications | Duration and side effects |
| Letrozole (Femara)
Anastrozole (Arimidex) Exemestane (Aromasin) |
Aromatase inhibitors (AIs; stop most estrogen production by blocking the aromatase enzyme) | Mainly for post-menopausal women with treated early-stage breast cancer
Lower the estrogen level Slow the growth of the cancer cells Prevent cancer from coming back Oral. Taken once a day |
2 to 5 years
Hot flashes Vaginal dryness Bone and joint pain Muscle pain |
Medications That Shut Down the Ovaries (Ovarian Suppression)
| Medications | Types | Indications | Duration and side effects |
| Goserelin (Zoladex)
Leuprolide (Lupron) |
Luteinizing hormone-releasing hormone (LHRH) agonists (stop the signals sent to the ovaries to produce estrogen) | For pre-menopausal women
Stop the ovaries from producing estrogen. The ovaries should start working again after therapy discontinuation Injectable. Given alone or with other hormone medications (Tamoxifen, Fulvestrant, aromatase inhibitors) |
5 to 10 years
Symptoms of menopause (temporary): hot flashes, night sweats, vaginal dryness, and mood swings |
When Should You Take Hormone Therapy for Breast Cancer?
After Breast Cancer Surgery (Adjuvant Therapy)
You can take hormone therapy for breast cancer after surgery to help reduce the risk of breast cancer recurrence.
Research shows that women who get at least five years of adjuvant therapy after surgery for early-stage breast cancer have lower risks of breast cancer recurrence and can live longer, up to 15 years.
Before Breast Cancer Surgery (Neoadjuvant Therapy)
Hormone therapy for breast cancer can also shrink a tumor before surgery, increasing the chance that surgery can entirely remove the cancer.
A shrinking tumor means you may only have a less complicated operation. Hormone therapy may also be necessary when surgery needs to be delayed or chemotherapy, which also helps shrink the tumor, is unavailable.
Can Hormone Therapy Prevent Breast Cancer From Occurring?
Yes. Most breast cancers are hormone receptor-positive, and trials have demonstrated the use of hormone therapy in preventing breast cancer in women with higher risks.
According to research:
- Tamoxifen lowers the risk of breast cancer by about 50% in post-menopausal women for at least 20 years.
- Some aromatase inhibitors reduce the risk of breast cancer by 50-65% in post-menopausal women for 3-7 years.
Depending on your condition, you may undergo multiple tests to keep track of your health and look for cancer progression or recurrence while receiving hormone therapy for breast cancer. Your doctor may adjust your treatment based on the results of these tests to determine how you respond to the treatment.
Yunique Medical provides FUNCTIONAL MEDICINE for optimized health and performance. We offer customized, scientifically advanced treatments to create a new state of human thriving. Why be ordinary when you can be optimal?
HUMAN 2.0 begins here!
Contact us to schedule your FREE consultation at one of our three locations in Florida – Ocala, Fruitland Park (The Villages), and Daytona.
UP NEXT: